Medical adherence, in simple words, means following the guidelines of your medical prescription strictly. In all types of illnesses, medical nonadherence plays a significant role in the healing process, especially in cases of chronic diseases.
According to a WHO study chronic illness is the leading cause of deaths nowadays, amounting to 73% of the total death count. To add more to the fire, 50% of the patients do not take medicines as per the prescription.Therefore, improving Medication Adherence, in general, has a far greater impact on public health than improvement in any specific treatment.
Medical Nonadherence And It’s Implications
NCBI defines medication adherence as the ratio of number of pills absent in a given period of time to the number of pills prescribed by the physician, which is converted into adherence percentage. A patient is considered to be adherent if the percentage is 80% or above.
Poor medical adherence, along with increasing probability of the morbid outcome, increases the estimated cost incurred with healing. As per a study conducted by WHO on cardiovascular diseases, these costs amount to $100 billion per year. Overall, this decreases the quality of life in patients while upping the risks of complications related to those diseases.
Adherence Challenges
Medication adherence can be a complicated process to get a grasp of. It depends on numerous factors throughout the course of care. These factors are related to the patient, supplier, treatment type, and healthcare system. They can be classified as the following categories for easier understanding:
i. Patient-Related
Most of the patients do not have a sufficient understanding of their diseases to follow a strict yet beneficial medical adherence. This is also affected by the general lack of medical literacy. In many other cases, patients are not fully involved or invested in the decision making process regarding their health plan. Patients are often biased towards certain medical procedures due to their existing beliefs based on previous experiences or anecdotal evidence. Patients’ loss of motivation during the course of treatment for their chronic illness also triggers medical nonadherence. In developing countries, there are several other factors like low socioeconomic status, inability to pay for medication, and lack of transportation that adds to the overall nonadherence.ii. Physician-Related
Most of the doctors aggravate the nonadherence by prescribing a complicated regimen of drugs to patients. They often fail to explain the severity and adverse effects of not following the prescription. Not understanding the financial burden of a patient, doctors prescribe an expensive therapy plan to a chronic illness ridden patient who can’t possibly follow it for a prolonged period. Lack of communication between a care provider and a patient causes this barrier that effectively lessens the adherence in patients. Studies have shown that less than 20% of the doctors directly communicate with their patients in the case of the first hospitalization.iii. System-Related
A broken health care system affects the adherence by not allowing a lot of patients the ease with which they can afford or access their prescription plans. Poor technological availability for health-related information means that the doctors can’t effectively communicate with patients regarding their adherence issues. Our health care systems are often overburdened with a large volume of patients being catered to by a single physician. This leads to less communication and poor assessment of patients. The system largely affects the time spent between a care provider and a patient which in turn, acts as a knowledge barrier.Ways Through Which Healthcare Providers Boost Medication Adherence

Non-adherence is a huge problem for health care providers as it affects them financially through various processes like unaccounted medicines, prescriptions going to waste, and a lot of other factors, without actually curing the patients in the long run. Using technology to boost medical adherence is a promising step in the right direction.
-
Leveraging the Internet of Things (IoT)
Studies report that people who use digital activity trackers to monitor their health are more likely to follow medical adherence. Healthcare providers are promoting the use of digital trackers in patients for the same reason. Tracking app manufacturers are also adding more ways for patients to follow their prescriptions. Apple is adding a medical adherence app in its Apple watch that helps senior users remember their prescription dosages on a periodic basis in the form of nudges or reminders.The tracking tech also affects adherence by introducing gamification to tap into the psyches of patients of all ages and demographics. Psychologically, humans are wired to prefer instant gratification over longer-term rewards. Companies like HealthPrize Technologies use this strategy to improve motivation in patients by supporting their good habit changes. They achieve this by employing different methods like videos, quizzes, surveys, etc. to bring about positive reinforcement. HealthPrize has a user base of over a million patients, which speaks volumes of their success.
-
Patient Education
The biggest patient-related barrier to adherence is a lack of knowledge. Health care providers counter this by conducting various seminars, informative workshops to increase awareness of medication adherence and how it reduces costs and time expenditure. Additional counseling with medicinal informative pamphlets has improved medication adherence in patients significantly as per the study conducted on patients with rheumatoid arthritis.Improving medication adherence on a large scale is a twofold process. The first step involves involves communicating the knowledge of the diseases via thorough discussions at every visit to the doctor. On the other hand, the second step is helping patients to overcome educational barriers by reminding them of taking medicines as prescribed. Cigna’s CoachRX service provides members with such educational resources. Members can also get daily reminders through different channels such as text messages, voicemails, or emails according to their preferences.
-
Providing a Guided User Experience
A guided user experience in a patient’s healthcare journey simplifies the process. Patients keep in touch with their healthcare providers through digital tools and sticking to their prescription is far more likely for patients who use these methods. This saves the healthcare providers’ costs of readmission and relapses. It also serves the other purpose of educating the patients to overcome the barriers related to medical literacy. United Healthcare uses digital tools to help members use their healthcare system. These include the selection of health plans based on users’ health and cost preferences, integration of payment apps such as Apple Pay, and personalized video explanations to clearly grasp policy coverage.
Digital Tools For Improving Medication Adherence
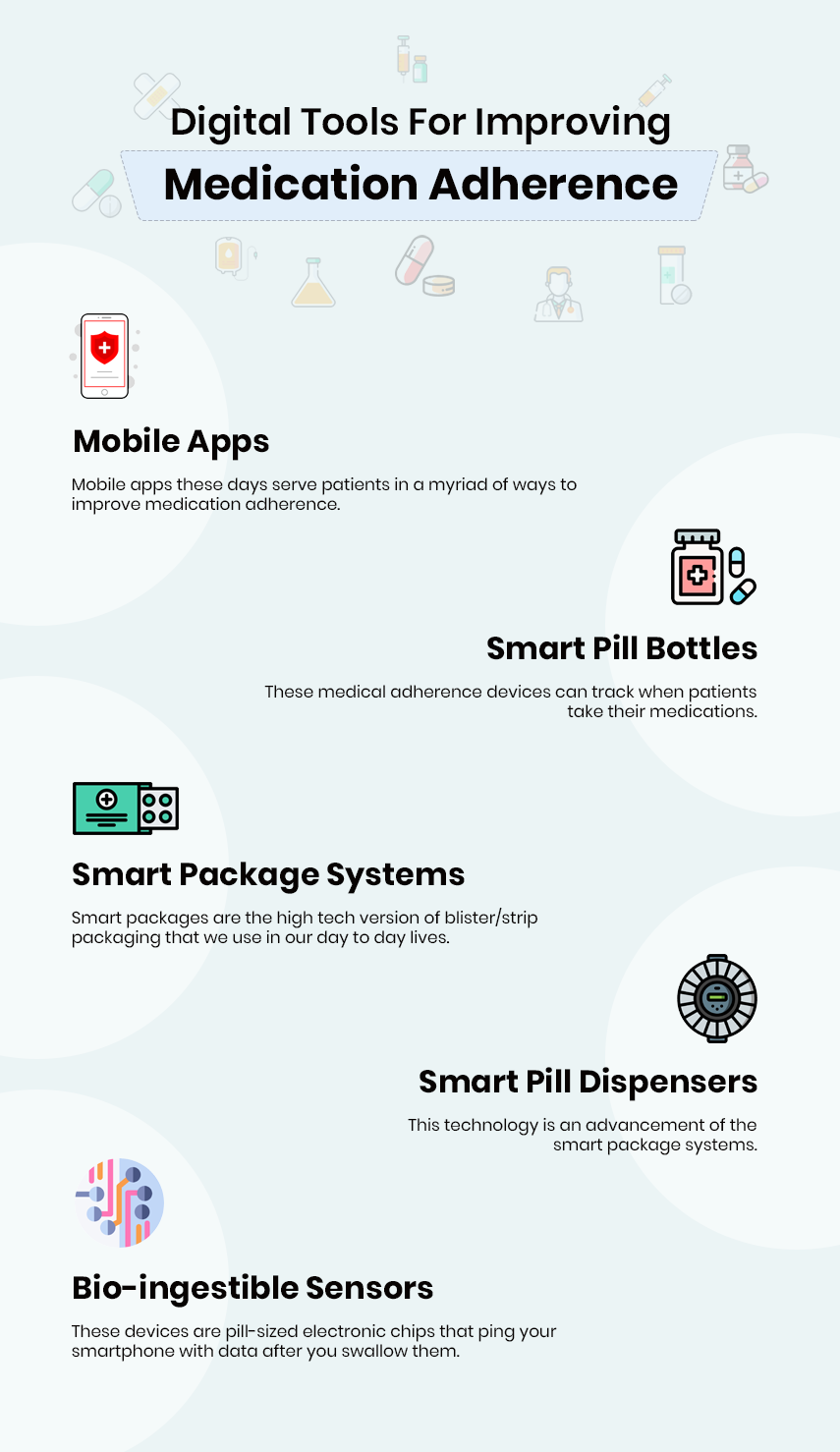
1 Mobile Apps
Mobile apps these days serve patients in a myriad of ways to improve medication adherence. Systems like Nomi collect patient data and identifies patterns. The system sends text messages directly to patients as a reminder prompts to take medicines. Other systems also allow healthcare providers to monitor patients between visits. It compiles patient-reported data, identifies symptoms, and connects to clinicians with the relevant data. Another similar product, Drive, streamlines the patient education and adherence programs. It uses gamification tools, behavioral psychologies, and loyalty marketing to improve medication adherence.
2 Smart Pill Bottles
These medical adherence devices can track when patients take their medications. It is done either through sensors in the bottle cap that detect when a bottle is opened or through sensors in the bottom of the bottle that can identify the weight of the pills and calculate if the patient was adherent. Smart bottles come with apps or as standalone products. One caveat is for patients who take multiple medications. The cost of smart bottles can go up fast in those cases. These devices can track when a pill is taken from inside, but they cannot correctly identify whether the medication was taken by the patient. Smart pill bottles sold by companies such as PillDrill, EllieGrid, AdhereTech, and others are designed to remind patients of their medication courses and makes significantly improves their adherence to the courses.3 Smart Package Systems
Smart packages are the high tech version of blister/strip packaging that we use in our day to day lives. These packages remind patients to take meds by alerting patients via sound cues and provide tracking of dispensed medicines. Unlike smart pill bottles, smart packages are advantageous for patients who are on multiple medications as they can be the ‘one-stop’ solution. These package systems also integrate with pharmacies in packaging and sending out their drugs. But as a downside, smart packages can be very expensive. Just like smart pill bottles, tracking if a pill was removed is possible but making sure the pill was taken by the patient, is not. Health provider Kaiser Permanente uses smart package systems to improve medication adherence.4 Smart Pill Dispensers
This technology is an advancement of the smart package systems. Like Apple’s Siri or Amazon’s Alexa, these devices use home voice assistants for their optimal outcome of medication adherence. These devices also incorporate remote access to medical professionals, and various other activation systems while dispensing meds. Just like smart package systems, smart pill dispensers tend to be quite expensive. Yet, they do not improve on the limitations of other systems like the medicines being dispensed but not being able to make sure they were taken by patients. RxPense is a smart pill dispenser for blister packaged medications, that is specifically designed for seniors and chronic disease patients.5 Bio-Ingestible Sensors
These devices are pill-sized electronic chips that ping your smartphone with data after you swallow them. They alert a patient’s on their smartphone and in some cases physician, with relevant data once they are in the patient's digestive tract. The patients will wear a patch on them to relay this data from the sensors. The first FDA-approved drug with a bio-ingestible sensor, Abilify Mycate, was introduced in November 2017. These sensors improve on other techs by actually being able to track adherence, but boosting adherence is still based on other factors. These devices are still a novelty in the market, and their real-world costs remain uncertain.
Digital Technologies Making An Impact

Medication Adherence with Digital Health is advancing in leaps and bounds with latest technologies being utilized. The improvement of compliance they achieve is backed with data evidence. Even though Medication Adherence technologies are still in the early stages, they benefit patients by boosting the efficacy of their meds and helping them avoid the danger of skipping/doubling prescription dosages.
Mobile apps like Nomi have shown to change patient’s behavior in 40% of the cases. The medication adherence tools of HealthPrize, which were slow to pick up at first, have now reported a notable improvement due to their facilitation in treatments and delivery methods across various demographics in the USA.
A Web-based prototype of the eHealth app—MIK—was co-designed with health care professionals and patients. The test done across hospitals with the data gathered from this app has shown that it has the potential to improve collaboration between doctor and patient.
Specific tools like Adherium's sensor, which snaps onto asthma inhaler, gives health care providers feedback on their patients. In a study done with children, preventive medication adherence rose up by manifold when this system was used.
Future Scope Of Medical adherence
Technology, on its own, is not a solution to the complicated matter of adherence, and that's because it doesn't work in isolation. Human intervention is required on all the techs. Smart pills, bottles, and packages only monitor dosages but the true adherence requires behavior change. On the first level is taking the medication correctly and another level is using the medication adherence devices optimally. Results are greater when the technology works with normal human behavior rather than working against it. The future of medication adherence lies in the effort on both the human side of this equation. On the patient side, it will have to facilitate more awareness of the importance of sticking to the prescriptions. On the health care provider’s side, it will have to bridge the gap of education of the health plans and medicines given by physicians to the doctors.
eHealth medication adherence tools are transforming every step of the patient’s healthcare path. From appointments, consultation, decision-making, medication dispensing, information acquisition and monitoring, to learning about medicine management in day to day life. eHealth can impact medication management at all three levels: healthcare systems, clinics/ pharmacies, and individual patients/carers. With the prevalence of IoT, information on doctor consultations, medicine prescriptions, and medication refills can be integrated into a centralized system. The access granted to the clinicians for this system can lead to improved overall experience for patients and healthcare providers.
Conclusion
Science of behavioral health goes back at least 70 years and has many proven theories on how to improve adherence. However, the challenge of medication non-adherence is deeply rooted in the psyche of patients.
A former U.S. Surgeon General C. Everett Koop has also said that drugs don’t work in patients who don’t take them.
But believing that the “fault” lies squarely with patients is a fairly destructive view of the problem. People generally understand how important medication is but forming habits to take them regularly is troublesome. Good and rewarding Habit-forming is the key solution. More and more app developers and healthcare providers understand that the best route to healthier people and lower costs is to encourage patients to form habits rather than preaching them to take their meds.
The end goal is for people to be so habitual that following medication adherence is effortless. Advanced technology coupled with the human intervention will truly improve the complex puzzle of medication adherence.






 December 31, 2019
December 31, 2019


